Introduction
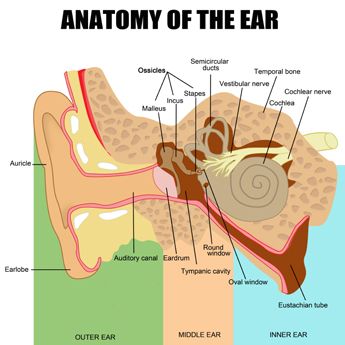
Vestibular schwannomas (also known as acoustic neuromas) are benign tumours that arise from the hearing and balance nerve, formally known as the vestibulocochlear nerve-the 8th cranial nerve. They actually arise from the balance (vestibular) component of this nerve, and specifically from the lining cells of this nerve, known as Schwann cells, hence the name-“schwannoma”.
Some anatomical considerations - where do they arise?
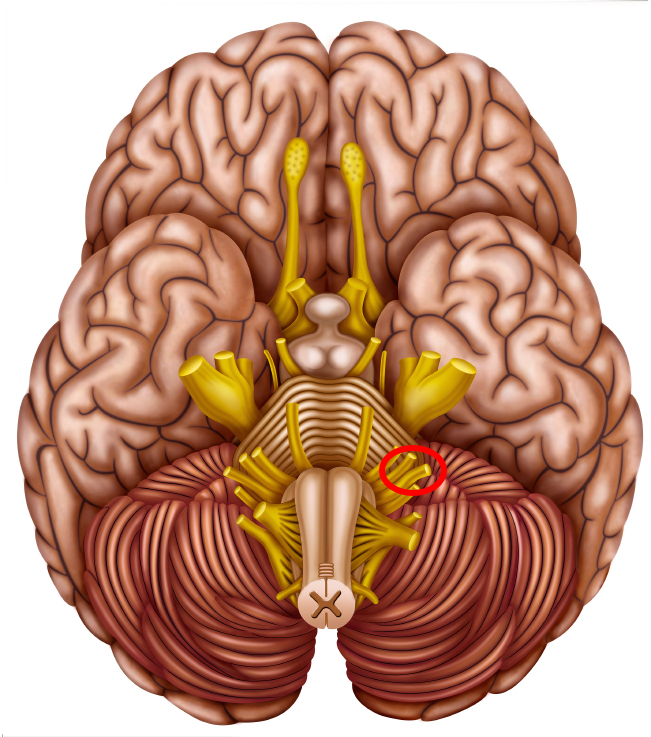 This picture shows the base of the brain with the cranial nerves emerging from it. The hearing and balance nerve is circled.
This picture shows the base of the brain with the cranial nerves emerging from it. The hearing and balance nerve is circled.
How do they present?
Vestibular schwannomas almost always occur as an isolated tumour with no specific risk or predisposing factors. They will usually start growing on the hearing and balance nerve within the internal auditory canal, a narrow canal on the inner aspect of the skull. Due to the confines of this canal, these tumours can cause dysfunction of the hearing and balance nerve whilst still very small (a few millimetres in diameter), and will typically present with hearing loss, tinnitus (abnormal sounds or ringing in the ear), or problems with balance.
Occasionally due to minimal or overlooked symptoms, vestibular schwannomas can go undiagnosed for many years and present when they are significantly bigger. In this situation they have usually grown out of the internal auditory canal into the brain cavity (a region known as the cerebello-pontine angle), and will start to compress the adjacent brain (the cerebellum and brainstem). If brainstem compression is significant, this can cause unsteadiness and clumsiness of the limbs. Other symptoms that can arise from vestibular schwannomas include altered facial sensation, hydrocephalus and swallowing difficulties.
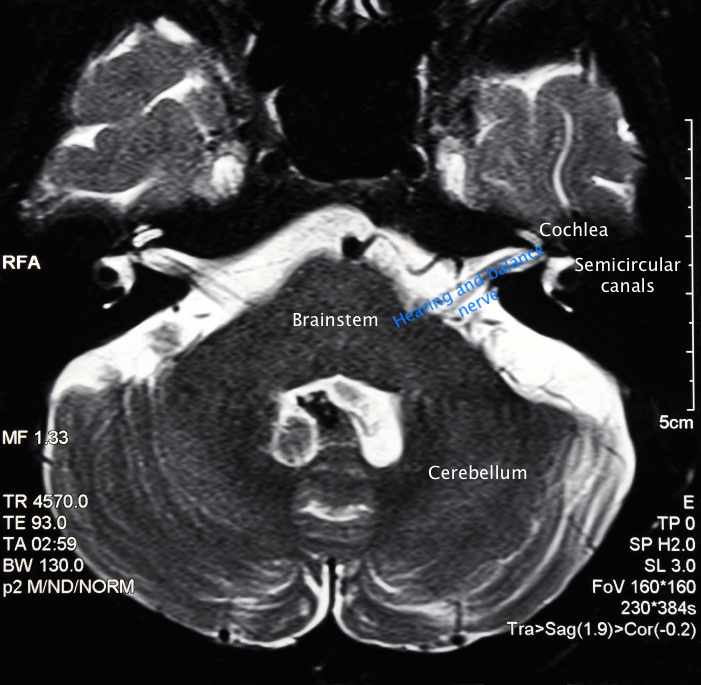 This scan shows a horizontal cross section through the brain at the level where the hearing and balance nerves run from the inner ear to the brain.
This scan shows a horizontal cross section through the brain at the level where the hearing and balance nerves run from the inner ear to the brain.
What are the management options?
The growth pattern of vestibular schwannomas is very variable. Up to 60% of them do not exhibit growth after being diagnosed, even though they must obviously have grown at some point in order to present. For this reason, they can often be safely monitored without any intervention for many years on end. This will only be the case for small and medium size tumours without any significant brain compression
The “watch, wait and rescan” management option is recommended in the majority of people with a newly diagnosed vestibular schwannoma. The characteristic regime of repeat MRI scans for monitoring a vestibular schwannoma is as follows:
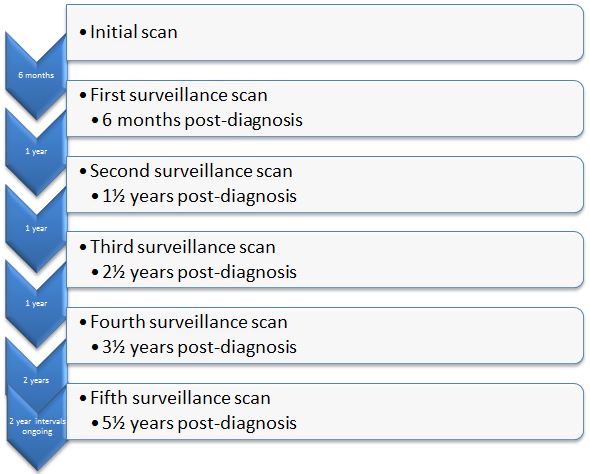
If a tumour remains static, then it is very likely that it will simply remain on this surveillance regime. If there is growth, then a decision will be made as to whether active treatment should be pursued, or whether further surveillance should be undertaken to ensure that the growth is persistent. The size of the tumour will be an important factor in this decision. The treatment options are covered in greater detail in the treatment section of the below.
Whether or not a vestibular schwannoma is growing may have little effect on the severity or progression of symptoms. This is particularly true for hearing loss and tinnitus. If you still have useful hearing in the affected ear, your surgeon will have an in-depth discussion with you about which management strategy is likely to offer you the best chance of preserving your hearing.
The management of your tumour will not only be discussed between you and your surgeon, but also at a Skull Base Multidisciplinary Team (MDT) Meeting. These are held fortnightly at Salford Royal Hospital, with a team of experts with a huge combined experience of managing such problems. Your surgeon will convey the outcome and recommendations of this meeting to you. Whilst this will provide you with all the information you require about your vestibular schwannoma, as well as a detailed analysis of the advantages and disadvantages of all management options, the most important factor in the final decision is you. Your personal opinion of what is best for you is undoubtedly the most relevant aspect of how you will be managed.
 Acoustic Neuroma
Acoustic Neuroma
Vestibular schwannomas treatment
As has been described in the section above, vestibular schwannomas, it is important to appreciate that perhaps the most common treatment of a vestibular schwannoma is to simply monitor it with serial scans over the years, the so called “watch, wait and re-scan” option. The logic to this treatment option is that up to 60% of vestibular schwannomas do not grow. The reason for this is not well understood, particularly given that they have presumably grown at some point in order to be present at the time of diagnosis. Intervention for a vestibular schwannoma is based either on evidence of growth or that, on initial presentation, the vestibular schwannoma is of sufficient size that it is considered unsafe to not intervene. The 2 treatment options for those vestibular schwannomas that require intervention are microsurgery and stereotactic radiosurgery.
1) Surgery
Surgery is aimed at the physical removal of the tumour and, therefore, cure of the condition with decompression of any of the vital structures upon which the tumour presses. It is a very effective treatment option but it is essential that the surgery is carried out by a surgeon with proven expertise. In our opinion, this level of proof requires participation in the national audit programme run by the British Skull Base Society and the scrutiny of international colleagues by publication in peer review journals. The skull base surgeons at The Brain and Spine Clinic, Scott Rutherford and Andrew King, actively subject themselves to this scrutiny of their surgical results.
As has been described, the surgery in principal is straightforward. It involves the physical removal of the tumour without harm to the adjacent structures the most important of which is the facial nerve. It is an accepted fact that the ability to preserve facial nerve function and thereby avoid producing a post-operative facial paralysis relates to the skill of the surgeon. Scott Rutherford and Andrew King are firmly committed that this skill needs to be more than simply an assumption but rather something that is proven by regular publication of their results as described before. They are both nationally and internationally recognised for their skill in this surgical field.
Surgical Approaches
Within the obvious parameter that the purpose of the surgery is to remove the tumour there are 2 different surgical routes to access the tumour as it lies within the head. These are the translabyrinthine route and the retrosigmoid route. In the right hands, both are able to produce excellent results.
Our standard route for approaching vestibular schwannomas is the translabyrinthine route. This offers excellent tumour exposure and in our hands maximises the chances of preserving facial nerve function. The alternative route is the retrosigmoid approach. Whilst the translabyrinthine route is our more routine approach, it does not offer the possibility of hearing preservation. We use the retrosigmoid approach is used in the relatively small number of patients with good hearing and in whom the surgical anatomy, as defined by the pre-operative MR scan, lends itself to the potential of hearing preservation surgery.
There is no doubt that even in the hands of expert surgeons, the surgery is a major undertaking and there are risks associated with this. These will be discussed in clinic with your neurosurgeon. Please be reassured that the complication rates are low but do include the following:
- Temporary or permanent facial weakness (our facial nerve outcomes are elaborated upon below).
- Injury to other nerves in the vicinity of the tumour. This could result in facial numbness, swallowing problems and/or double vision. Commonly, even on the rare occasion when this occurs, it will be due to the surgery itself and will therefore be temporary.
- Hydrocephalus
- Leakage of cerebro-spinal fluid (CSF) through the surgical access route. CSF is the clear, watery fluid that bathes the brain. It does not clot like blood, and so will potentially leak out of your surgical wound. This can result in CSF appearing either through the wound itself, or more rarely out of the nose (due to CSF escaping through the Eustachian tube which links the middle ear and the back of the nose). The risk from a CSF leak comes from bacteria in on the skin or in the back of the nose tracking back along the route of the leak and causing an infection within the head (meningitis). A CSF leak cannot, therefore, be ignored nor expected to resolve spontaneously. It requires prompt treatment which can involve reinforcing stitches in the skin and/or a diversionary drain being placed in your lower back to drain CSF through this route and thereby facilitate the wound sealing up again. Very occasionally a CSF leak requires a return to the operating theatre for a formal re-repair of the wound.
- Infection, either in the wound or deeper within the head. Infections can usually be treated very effectively with antibiotics provided that they are diagnosed and treated promptly.
- A very small risk of a potentially devastating complication inside the brain such as a stroke, a bleed or a serious infection. These are complications which are potentially life-threatening when severe (although the risk to life from this operation is less than 1%).
- Loss of function of the hearing and balance nerve. Loss of balance is inevitable as this is the nerve that the tumour has arisen from. However, a large number of people have already lost function before surgery and compensated accordingly. If function does remain before your operation, you will feel unsteady in the early days and weeks post-operatively, but then will steadily compensate for this loss of function. Hearing loss will be inevitable if the surgical route is translabyrinthine due to loss of the inner ear. If surgery is aimed to be hearing preserving, your surgeon will give you an individualised estimate of the chance of hearing loss occurring.
- Other small risks from the anaesthetic or related to a period of immobility such as chest infections or deep venous thrombosis.
Surgical results
As part of our rigorous process of surgical outcome review, we carried out a detailed audit of our vestibular schwannoma surgery results in 2013. This looked at results of all operations performed over a 6-year period from 2007 to 2012 inclusive. During this time we performed 292 vestibular schwannoma surgeries between us, often operating together for larger or more difficult tumours. We have divided the outcome measures according to the size of the tumour as assessed by the Tokyo Classification System. This measures the maximum dimension of the tumour within the brain cavity (the cerebello-pontine angle) and does not include the portion of the tumour within the internal auditory canal. The breakdown of grades according to size is as follows:
| Grade |
Description |
Size (mm) |
| 1 |
Small |
1 - 10 |
| 2 |
Medium |
11 - 20 |
| 3 |
Moderately large |
21 - 30 |
| 4 |
Large |
31 - 40 |
| 5 |
Giant |
> 41 |
Our results are as follows:
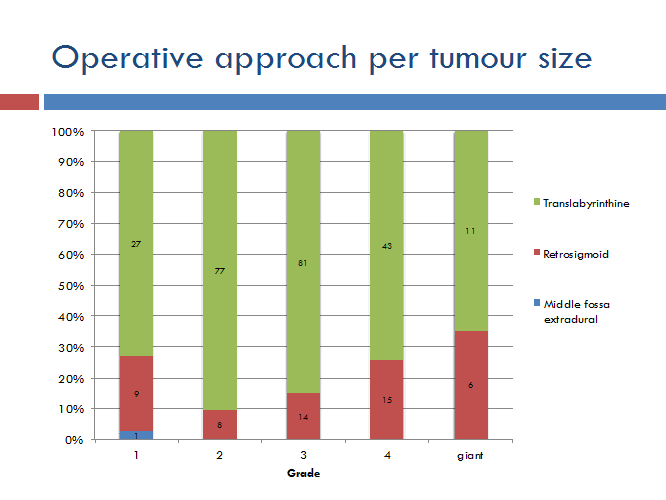
This graph illustrates the preponderance of translabyrinthine approaches.
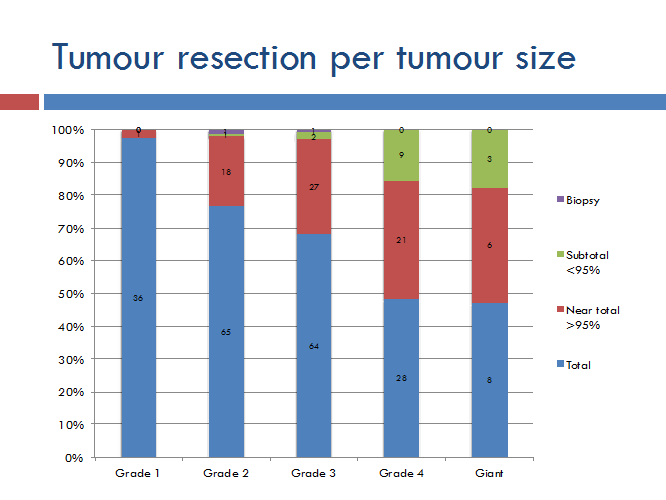
This graph shows the extent of tumour resection according to tumour size. This is a balance between maximal tumour removal to achieve long-term control or cure of the tumour vs. the risk of creating permanent harm to the facial nerve. A near-total removal means leaving a tiny fragment of tumour on the facial nerve because of its extreme adherence, and overall we still achieve >95% tumour removal. Subtotal removals refer to a tumour remnant larger than 5% of the original size, and this is rarely performed in very demanding tumours or where the patient cannot withstand prolonged surgery. Even with near-total removals, approximately 75% of patients have no tumour remnant visible on follow-up scanning.
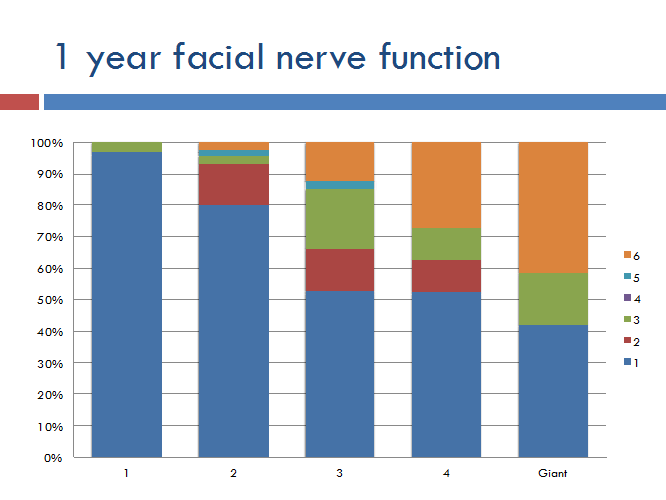
The facial nerve outcomes are graded according to the House-Brackmann (HB) grading system, which is a scale from 1 to 6 (shown on the right of the graph). On this scale, grade 1 is entirely normal facial function, grade 2 is very slight weakness and continuing up to grade 6 which is complete paralysis. This graph shows facial nerve outcomes according to tumour size, but does not take account of those patients with a pre-operative facial weakness. These results are illustrated below:
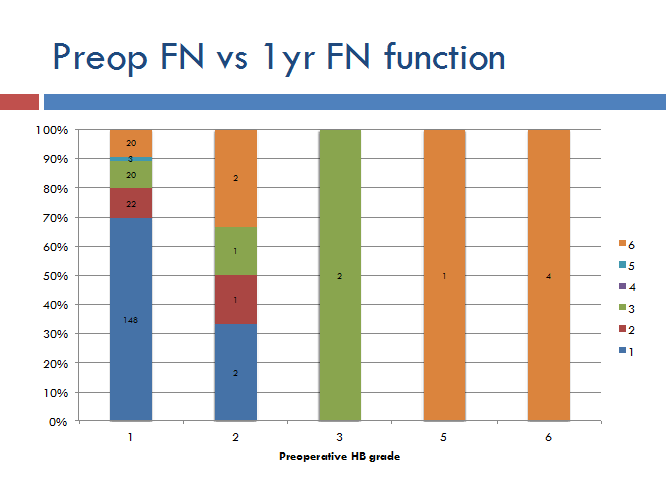
The relevant column is on the far left showing people with normal facial function before surgery (HB grade 1). This shows across all tumour sizes we achieve:
- 70% grade 1 facial function
- 80% grade 1 or 2 facial function
- 90% grade 1-3 facial function
Further details about surgery for vestibular schwannomas is contained within the leaflet from our practice at Salford Royal Hospital.
Surgery of Acoustic Neuroma
2) Stereotactic Radiosurgery
Introduction
Despite what the name would suggest, stereotactic radiosurgery is simply a form of radiotherapy. The stereotactic part of the name refers to the fact that it uses very precise mathematical modelling to target the radiotherapy dose to the tumour. The radiosurgery component refers to the fact that  this radiotherapy dose is delivered in a single dose, rather than multiple fractions of an overall dose which is more common for radiotherapy which is delivered for cancers.
this radiotherapy dose is delivered in a single dose, rather than multiple fractions of an overall dose which is more common for radiotherapy which is delivered for cancers.
Stereotactic radiosurgery for vestibular schwannomas is now a well proven treatment with a track record going back for at least 20 years. Whilst it does not remove or necessarily reduce the tumour, the treatment aim with stereotactic radiosurgery is halting growth and it achieves this in more than 95% of cases. We at the Brain and Spine Clinic feel that this is a very effective and safe treatment to be offered for a vestibular schwannoma.
Different types of stereotactic radiosurgery
Stereotactic radiosurgery is carried out using a variety of delivery methods. These are known by various names which include Linac, Novalis, Gamma knife and Cyber knife).Whilst there are a range of claims for whether one or another is best, there is no doubt that they are all highly effective and safe techniques for giving very accurate radiotherapy.
The risks of treatment are very low, although a small proportion of patients undergoing this treatment will develop facial weakness and/or facial numbness. These risks are typically less than 1 to 2%. A small number of patients can also develop brain swelling or hydrocephalus.
It is important to note that not all vestibular schwannomas are appropriate for radiosurgery. The main determinant is the size of the tumour, with larger tumours being less amenable to radiosurgery. The upper limit of size is not absolute, but typically, a tumour of more than 3 cm in diameter will not be offered stereotactic radiosurgery.
Stereotactic radiosurgery has a relatively high initial hearing preservation rate if your hearing is maintained prior to treatment. However, this does tend to deteriorate in the years following stereotactic radiosurgery. If you are considering this treatment, this will be discussed in far greater depth by your surgeon.
Given that stereotactic radiosurgery is designed to stop a tumour from growing, you will not be recommended this treatment unless your tumour has indeed been shown to be active. In the small number of cases where stereotactic radiosurgery fails to halt growth of the tumour, salvage surgery may have to be undertaken. Surgery in these circumstances is undoubtedly more difficult and produces poorer results, particularly with reference to facial nerve outcome.
Treatment choice is a complex decision and a highly individual one. You surgeon will you through this process and ensure that you are comfortable with any treatment choice you make.