The spine is a highly complex structure, both in terms of its role as part of the bony skeleton and the critical neurological structures that pass through it. This section is designed to give a brief guide to the most important anatomical aspects of the spine, both in health and disease. This will allow you to better understand some of the terms that are used elsewhere in this site to describe various spinal conditions.
Although the spine functions as one large complex unit, it is helpful to think of the mechanical (spinal column) and neurological (spinal cord and spinal nerves) aspects individually.
Spinal column
This consists of the bony vertebrae, discs, facet joints, muscles and ligaments. Together these structures fulfil a number of functions, which include supporting your head and trunk, providing a vast range of movement between one end of the spine and the other, acting as a shock absorber and protecting the nerves that run through the centre of it.
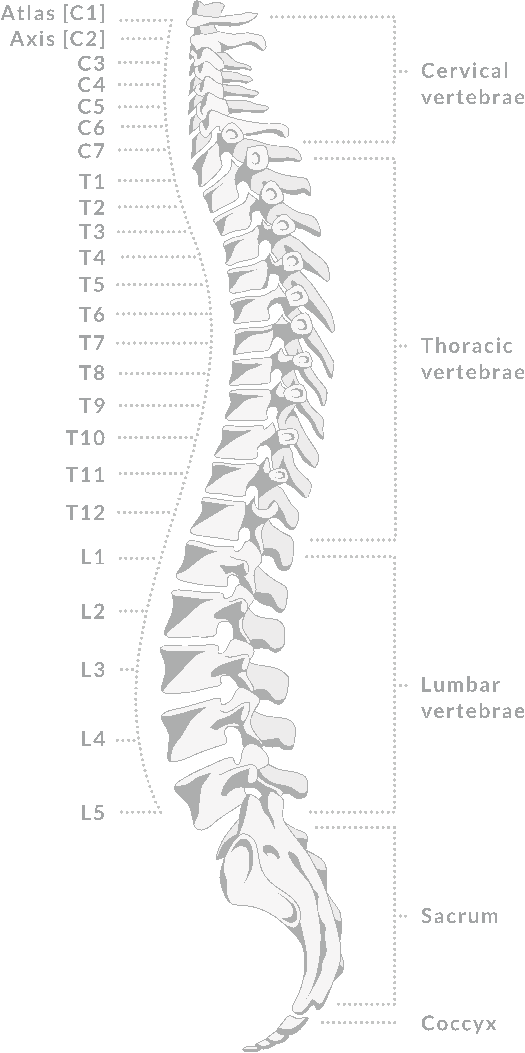
The spine is divided into 33 segments, 24 of which are mobile. Working from the top downwards, the cervical spine is the portion of the spine within the neck, and consists of 7 vertebrae (C1 to C7). The first two cervical vertebrae have a very specialised shape that allows most of the rotation of your head (side-to-side movement) to occur here. The 12 thoracic vertebrae (T1 to T12) are contained within the rib cage, and each vertebra articulates with a rib. These are far less mobile and this more rigid structure of the thoracic spine provides the necessary support for the vital organs contained in the chest (heart and lungs). The lumbar spine is the lowest mobile segment and is commonly referred to as the lower back. It has 5 vertebrae (L1 to L5), and these are the largest vertebrae in the spine as they have the greatest load to bear. As a result the lumbar spine is generally the area that wears the most. The lumbar spine articulates with the sacrum, which consists of 5 segments all fused together into 1 large piece of bone. The sacrum also forms the back part of the pelvis. Finally the coccyx or “tail” of our spine consists of 4 tiny segments all fused together.
It is normal for the spine to have a gentle “S” shape with the cervical and lumbar spine being concave and the thoracic spine convex. Maintenance of this shape is key to the health of the spine, and loss or accentuation of this curvature is a sign of underlying problems with the spine.

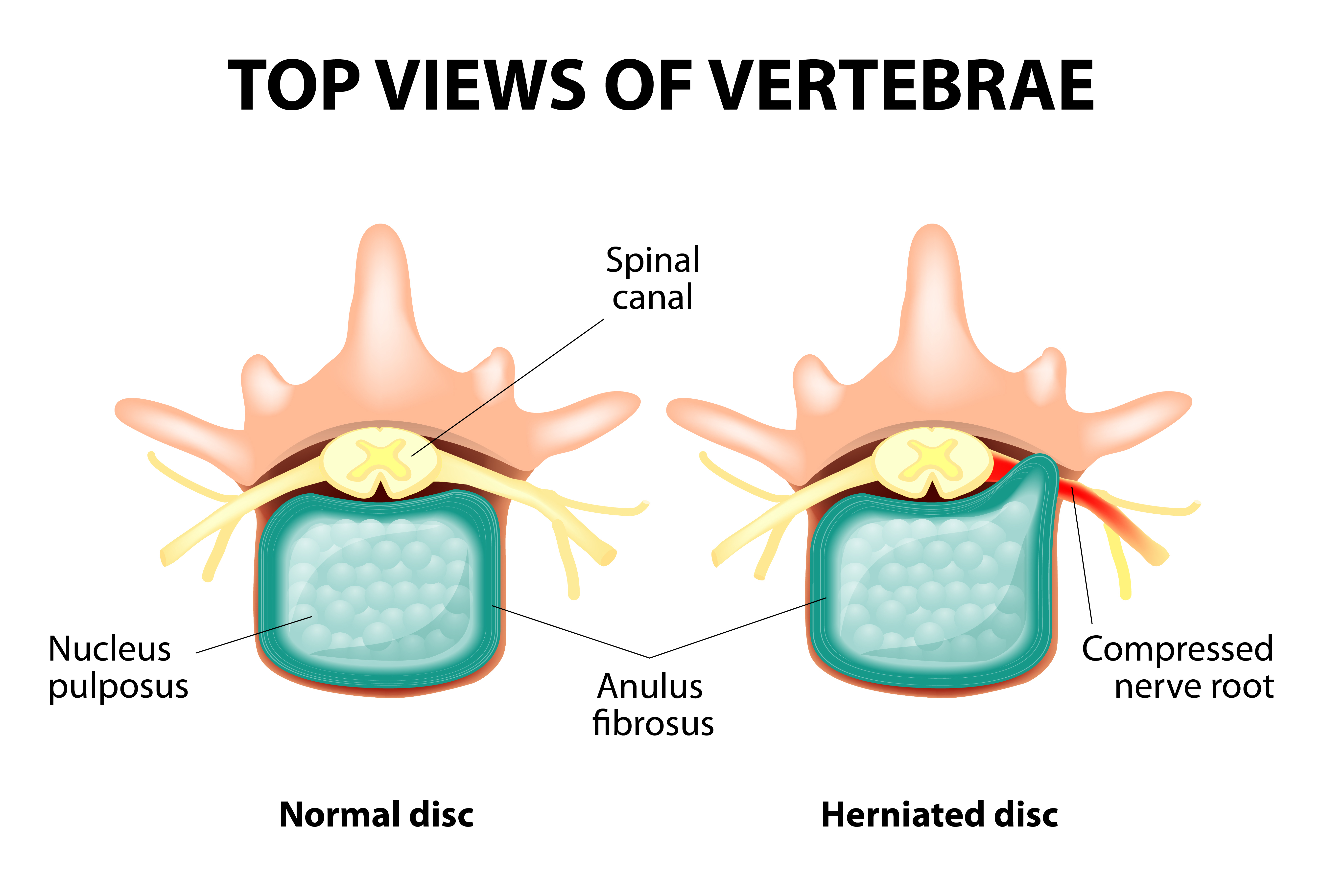
Between each vertebra are intervertebral discs. These are highly specialised joints that not only allow movement between adjacent vertebrae, but also act as a shock absorber. Discs are composed of two main parts. The first of these is the annulus fibrosus which is a tough fibrous capsule of concentric and criss-crossing fibres running around the circumference of the disc. The second part is the nucleus pulposus. This is a far softer material which provides the discs with its shock-absorbing properties. The process of disc wear is described in the disc prolapse section.
The discs are the joints between adjacent vertebrae at the front of the spine, but there are a pair of further joints between adjacent vertebrae at the back of the spine – facet joints. There is one pair articulating with the vertebra above, and one pair with the vertebra below, making four joint surfaces per segment. These joints are much like the majority of other joints in the body, and are known as synovial joints. They are lined by cartilage and contain lubricating fluid to facilitate movement. However, just as other synovial joints can wear, so can facet joints. The wear and tear process is very similar to that of a worn hip or knee; joint movements can become painful, the joint space becomes reduced and the joint itself can become enlarged. The pain from facet joint degeneration is often most pronounced with the back in extension (tilting back) or when it is straightening from a flexed position, as this is when there is increased pressure on the facet joints. The other problem that worn facet joints can cause is their enlargement can encroach on the space for the spinal cord and spinal nerves. This can then lead to the condition of spinal stenosis.

The muscles that surround and support the spine are frequently referred to as the core muscles. They can be divided into the muscles at the front of the spine for flexion of the spine (including the abdominal muscles) and the muscles behind the spine that extend it. The flexor and extensor muscles have an important role in maintaining the balance and the alignment of the spine, and when weakened, can lead to significant problems with mechanical back pain. Strong core muscles also help to reduce the strain on the spine itself. Maintaining healthy spinal musculature is therefore key to the overall health of the spine.
The other soft tissue components of the spine are the ligaments. These are tough fibrous structures which play an important role in stabilising the spine and keeping the vertebrae correctly aligned. There are three main ligaments which run from the top to the bottom of the spine (the anterior and posterior longitudinal ligaments and the ligamentum flavum), as well as further ligaments joining adjacent vertebrae such as the interspinous ligaments. As part of the degenerative process, ligaments can become enlarged or lengthened, and this can also contribute to the development of spinal stenosis or myelopathy.
Spinal cord and spinal nerves
The neurological part of the spine consists of the spinal cord and the nerves emerging from it (the spinal nerves). These are contained deep within the centre of the spine in the canal formed by bony arches of each vertebra. The enveloping bone and ligaments means that the neurological structures are exceedingly well protected.
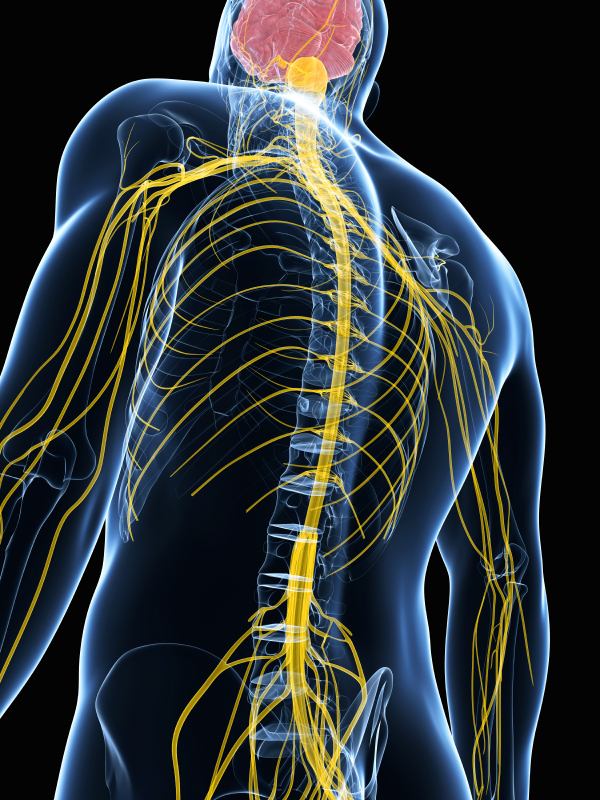
The spinal cord emerges from the brain cavity where it is continuous with the lower brainstem. It runs down to the level of the L1/L2 junction, where it terminates and becomes a collection of spinal nerves (the cauda equina), which will progressively exit from the spine at each successive level. The spinal cord carries a vast amount of information both to and from the trunk and limbs. The motor messages run from the brain downwards, and sensory signals originate peripherally and are then relayed back to the brain via the spinal cord. Considering the number and speed of the electrical messages conveyed, the spinal cord is a remarkably small structure only measuring approximately 12-14mm in maximum diameter.
The spinal cord is enveloped in a number of protective coverings called the meninges. The outer layer is the dura, which is the thickest and toughest membrane. Within the dura there are two much thinner membranes called the arachnoid and pia. There is a narrow space between the dura and the bone and ligaments of the spine, and this is called the epidural space. It is this space that is targeted for steroid or anaesthetic injections. On the inside of the arachnoid membrane, a clear watery fluid called cerebrospinal fluid (CSF) bathes the spinal cord. A lumbar puncture accesses CSF from this space, and a contrast dye can be injected into it when obtaining a CT myelogram.
Emerging from the spinal cord are 31 pairs of spinal nerves (8 cervical, 12 thoracic, 5 lumbar, 5 sacral and 1 coccygeal). These emerge from the spine though a small opening between adjacent vertebrae, called the intervertebral foramen. The nerves are numbered according to the segment of the spine from which they exit, for example C6 or L5. Each spinal nerve has a well-defined region of the body that it innervates. The motor (or muscle strength) distribution of a particular spinal nerve is called a myotome, and the sensory area that it carries information from is called a dermatome. Knowledge of myotomes and dermatomes is a helpful guide for your surgeon in localising the level in your spine that may be responsible for pain, weakness or sensory disturbance.